An awake intubation should be considered primarily if serious doubt exists about whether the clinician can easily take over the gas exchange a patient is presently doing for him- or herself. There are two broad categories of indications to consider awake tracheal intubation in an emergency:
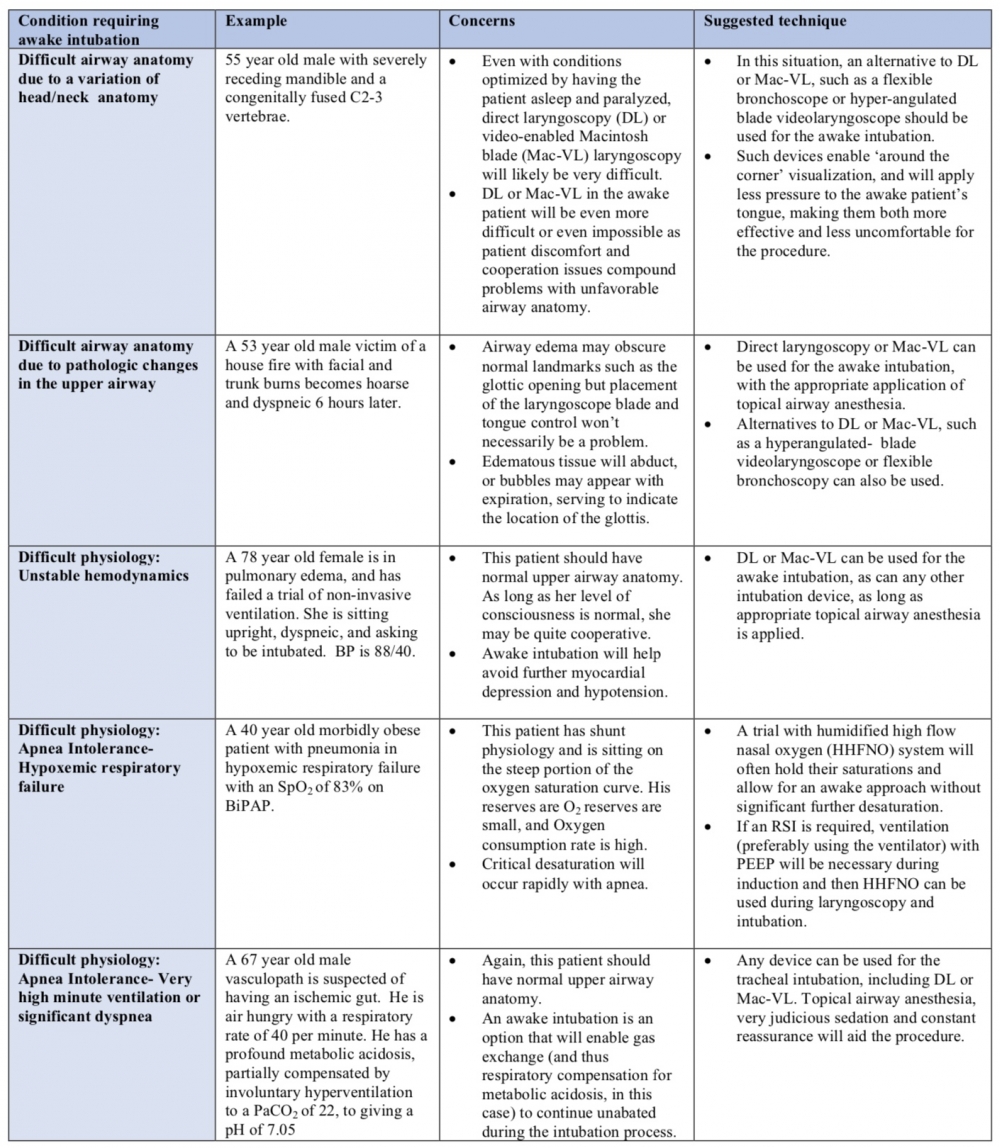
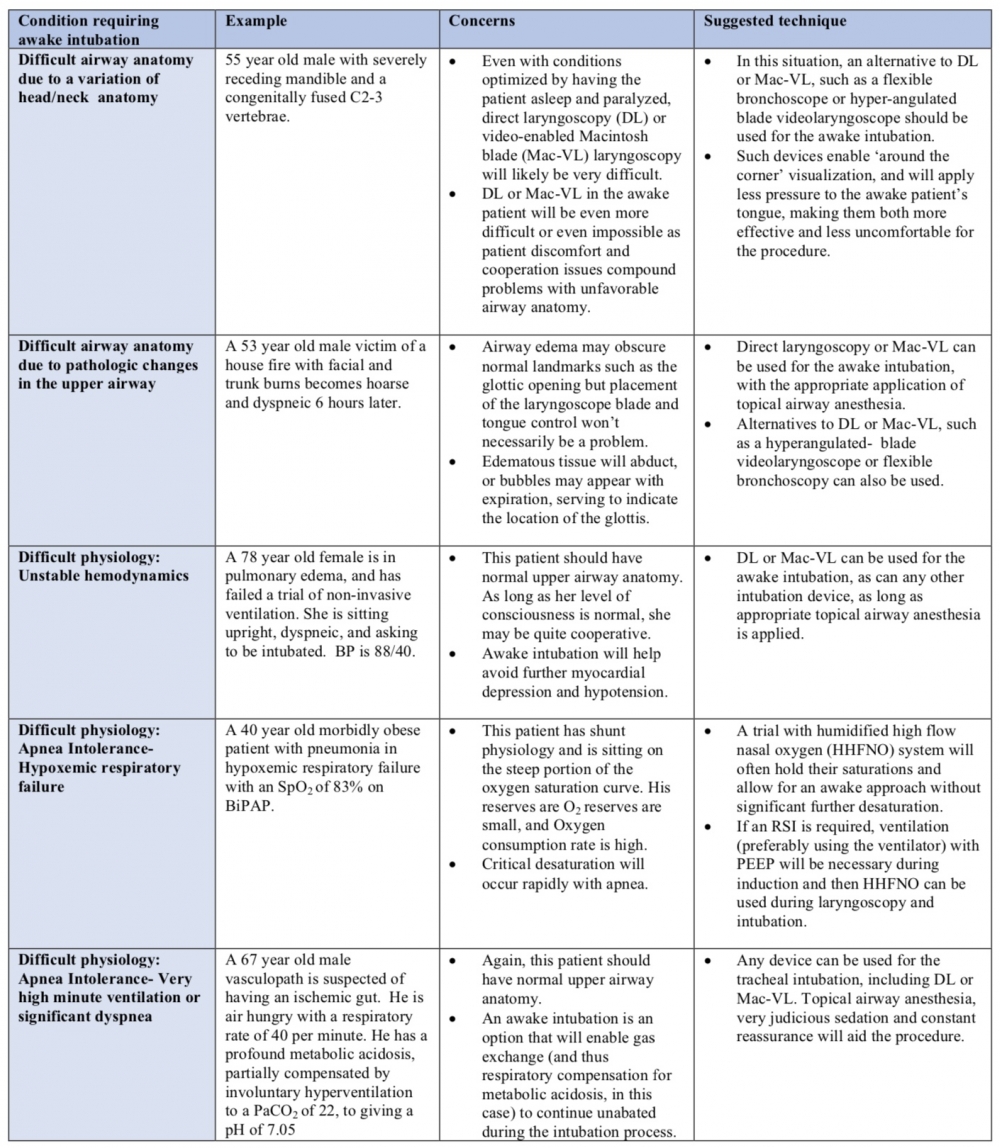
Predicted difficult airway anatomy. Awake intubation should be considered if difficulty is predicted both with tracheal intubation and maintaining oxygenation with face mask ventilation (FMV) or supraglottic airway (SGA) rescue ventilation should intubation fail. Two types of difficult airway anatomy can be described:
- Variations in normal head/neck anatomy: Some aspect(s) of the patient's usual anatomy predicts difficulty with tracheal intubation or the ability to accomplish effective ventilation by FMV or SGA;
- Pathologic airway distortion or obstruction: Difficulty is predicted based on de novo pathologic changes in the airway.
The distinction is important because as discussed in table 2, VL may be an option for awake intubation of some of the former group, while the latter group will often require flexible endoscopic intubation (FEI).
Predicted difficult physiology. Even with favorable airway anatomy, some patients present physiologic issues that may favor an awak intubation.
Hemodynamic instability: With significant hemodynamic instability, concern may exist over the effects of RSI induction agents on the blood pressure. While careful choice of induction agent and dose, together with a fluid bolus and/or the pre-emptive use of vasopressors and inotropic agents will often enable safe conduct of an RSI in this situation, an awake intubation is a second option to help maintain blood pressure during tracheal intubation.
Apnea intolerance: This can occur in two clinical settings:
-
- High minute ventilation: The patient who is extremely dyspneic on the basis of cardiopulmonary compromise or who is hyperventilating to compensate for a profound metabolic acidosis will tolerate interruption of gas exchange poorly. Early institution of FMV with PEEP and administration of high flow oxygen by nasal cannulae during an RSI is one option. Alternatively, an awake intubation will allow the patient to continue to manage his or her own gas exchange until the airway is secured.
-
- Hypoxemia: Patients with significant shunt physiology will be difficult to pre-oxygenate and their resultant small oxygen reservoir (the functional residual capacity, FRC), often combined with higher than normal rates of oxygen consumption will predispose them to rapid desaturation with the onset of apnea as part of an RSI. These patients will often desaturate very quickly despite apneic oxygenation. While assisted ventilation during the induction phase of an RSI may avert critical hypoxemia, clinicians may alternatively choose an awake approach with humidified high flow nasal oxygenation support during the procedure.
-